Bladder cancer is diagnosed in 80,000 people and is responsible for 17,000 deaths in the United States annually
Fortunately, most (70%) of new bladder cancer diagnoses are early stage (ie, Ta, Tis, and T1 disease and have not yet invaded the muscular layer of the bladder wall. These patients are often managed with transurethral resection of bladder tumor (TURBT) with or without the addition of therapeutic agents instilled into the bladder to reduce recurrence. The remaining 30% of patients have muscle-invasive bladder cancer, including cancer involving the muscularis propria (T2), perivesical tissue (T3), or adjacent pelvic organs/structures (T4).
Radical cystectomy (surgical removal of the entire bladder) is the historical gold standard treatment for muscle-invasive bladder cancer. Radical cystectomy (RC) often involves removal of the bladder (in combination with removal of the uterus/ovaries/fallopian tubes and possibly a portion of the vagina in women and the prostate and seminal vesicles in men), pelvic lymph node dissection, and reconstruction of the urinary tract.
Because of the high risk of distant failure in muscle-invasive bladder cancer, chemotherapy either before or after RC is often administered to improve outcomes. Patients managed with RC have a five-year pelvic control rate of nearly 80% and five-year overall survival rates ranging from 40-60%.
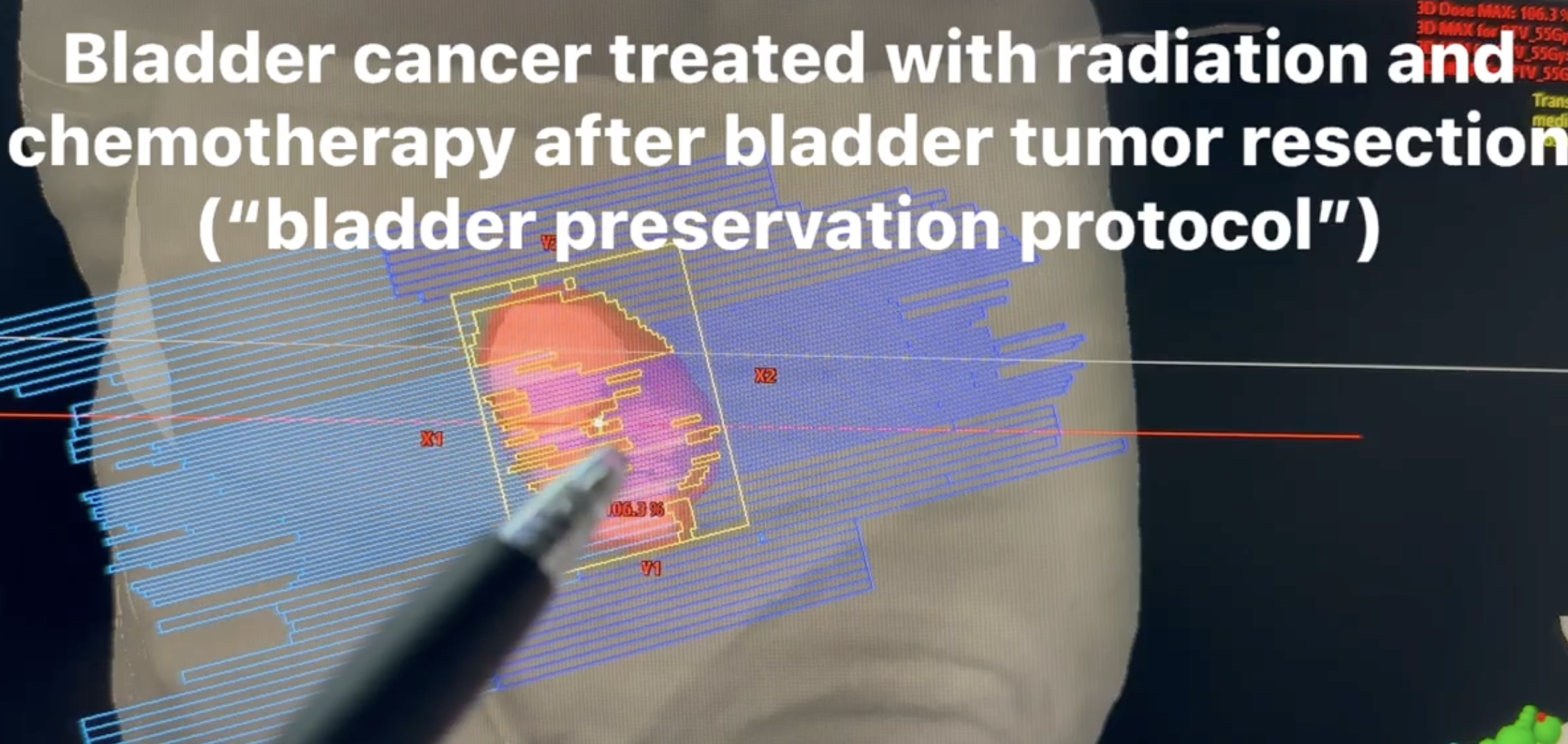
A non-cystectomy alternative is an option for well-selected patients with muscle-invasive bladder cancer who are either poor candidates for RC or patients who want to keep their bladder. This treatment is called trimodality therapy (TMT), which involves incorporating TURBT followed by radiation therapy (RT) with concurrent radiosensitizing chemotherapy. This treatment option preserves a functioning bladder This combined-modality approach utilizing TURBT followed by RT with concurrent chemotherapy is often referred to as trimodality therapy.
“Generally accepted criteria for surgically fit patients suitable for this approach include those with small (<4-7cm) unifocal tumors, well-functioning bladders, and an absence of obvious extravesical extension, carcinoma in situ, or hydronephrosis.”
“Data presented at the 2022 American Society of Genitourinary Oncology meeting where a multicenter retrospective 3:1 matched comparison analysis of TMT (n=282) and RC (n=834) showed no difference in 5-year metastasis-free survival between treatments (78% vs. 73%, p=0.07) and a statistically significant cancer-specific and overall survival advantage in those treated with TMT (85% vs. 78%, p=0.02, 78% vs. 70%, p<0.001). Moreover, only 13% of patients undergoing TMT required salvage cystectomy for treatment failure or toxicity which has been often touted as another reason to avoid TMT.”
Radiation therapy typically takes about 15-minutes/day, 5-days/week for 4-weeks. Chemotherapy is given during the treatment course. Side effects in the majority of cases are very well-tolerated.